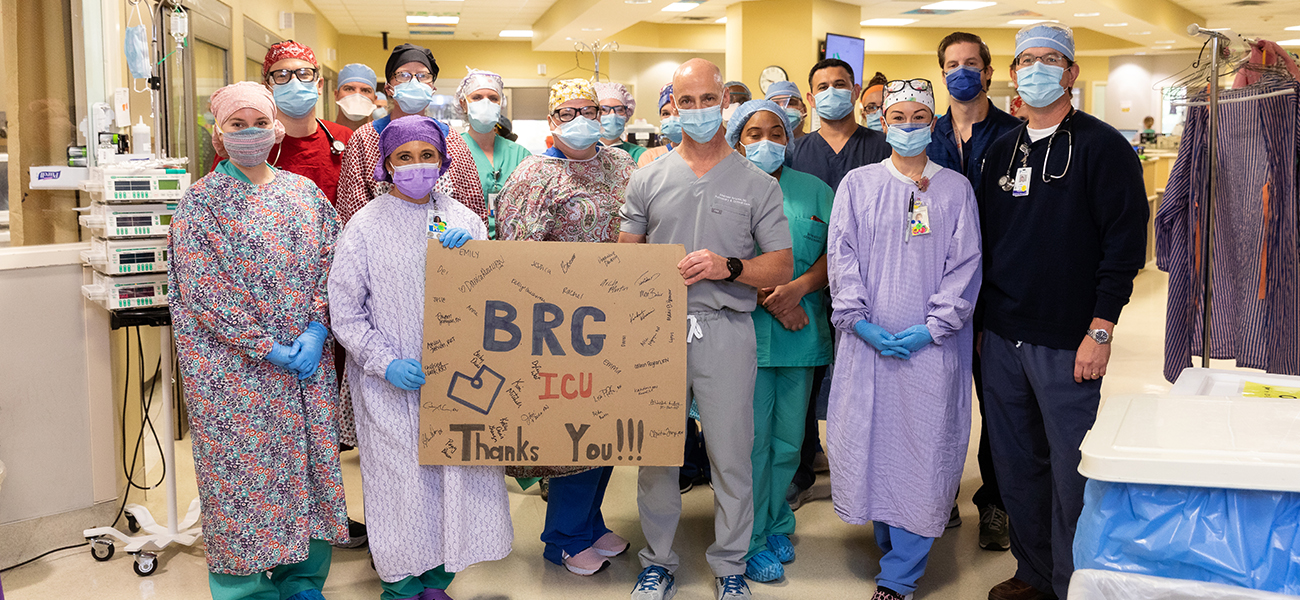
Fighting the virus might feel like a battle, but Baton Rouge General staff say they’re ready for the challenge
“I specifically recall the first two times I spoke with families of a COVID-presumed patient. I introduced myself; I let them know their loved one was stable and on a breathing machine. And each time the family member would ask, ‘Do you think this is coronavirus?’ And I would say ‘Yes, I do believe it’s coronavirus.’ The fear that response generated in the family was crushing. I’m a lung doctor. I tell some patients that they have lung cancer that has spread all over their body and that we’re not going to be able to cure it. But I have never seen fear like this in families.
We quickly had to change our messaging to decrease their anxiety. We built an iPad stand with an external speaker that we roll into the rooms. We FaceTime and explain to families what they are looking at in the room and what we are doing. And each day as we round on that patient, we call them in real time while we’re at the bedside.

|
|
The families have been wonderful. They are thankful every day. I spoke with 14 families today. And every one of them starts the conversation by saying, ‘How are you, Stephen?’
— Dr. Stephen Brierre, Pulmonary/critical care physician, Baton Rouge General
“During the peak of flu season, we may only see five or six patients who are super, super sick and are maxed out on ventilator settings. The majority of these patients that end up on the ventilator now—they’re all like that. It’s been like flu season on steroids.
It’s so hard to describe. It’s something I never thought I would be dealing with as a respiratory therapist.
Your patient load has increased, and you’re dealing with the sickest patients you’ve ever dealt with. We’re used to an average of eight to 10 ventilators in the ICU during normal times. Now, each therapist on their own is taking care of eight to 10 patients on ventilators, sometimes even 12.
When you have to intubate, it has to happen very fast because their oxygen levels drop very quickly. The other day, I started my rounds on the COVID unit with eight ventilators. And I couldn’t even see my first patient before two patients needed to be intubated, and we intubated two more patients back to back.
It’s very hard. You’ll have one patient that has passed away, but you can’t forget about your other eight patients who are on ventilators that you have to take care of. You literally go from withdrawing life support from one patient to the next one with your happy face on.
It’s like a war zone. It’s like the Wild West. You never know what’s coming. We’re working extra shifts. It’s emotionally, physically and mentally exhausting on all ends. But somehow, we just keep going.”
— Ashley Joffrion, Respiratory therapist, Baton Rouge General
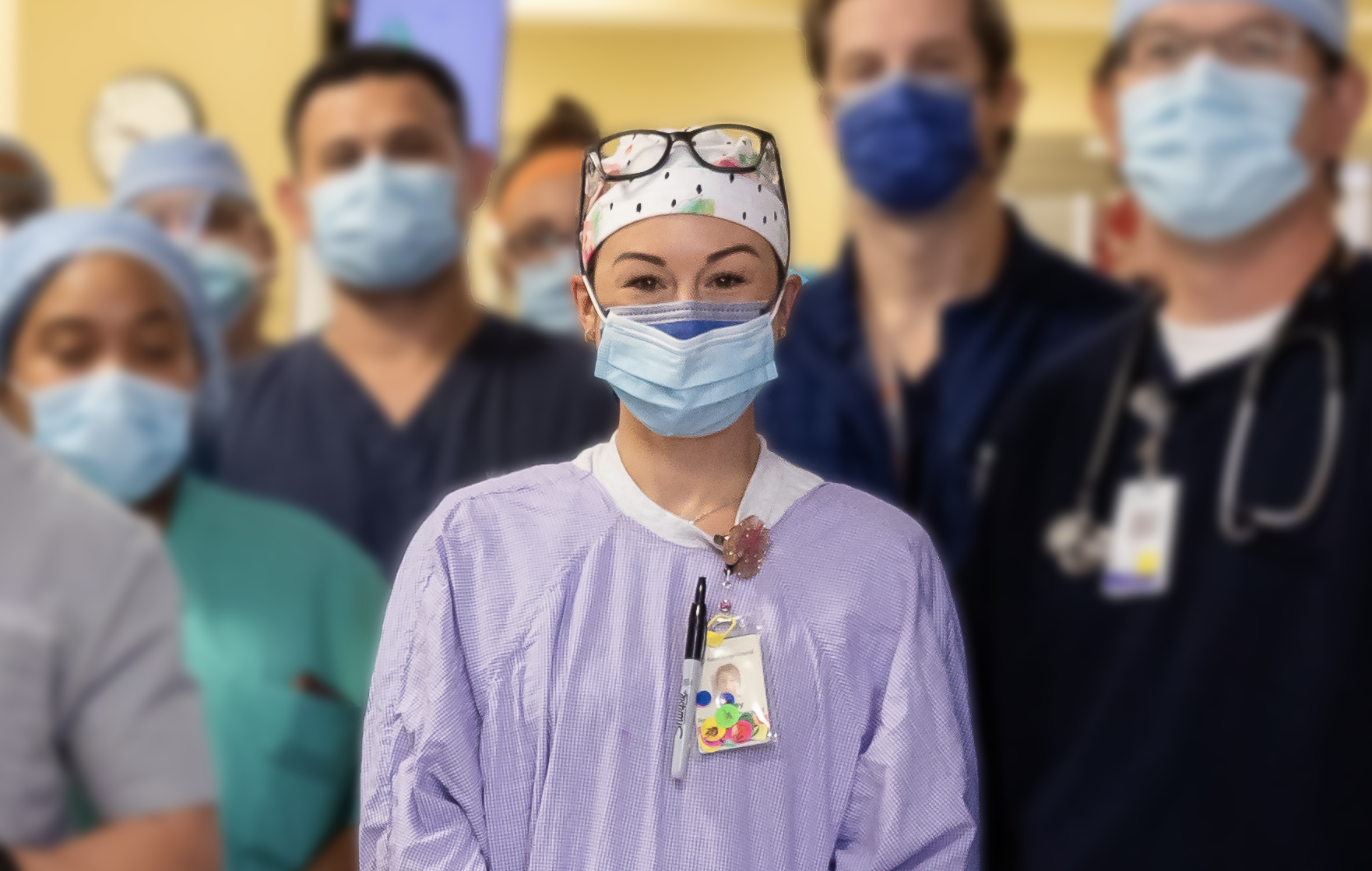
In nursing, you’re in a very unique position to love and care for people. It’s pretty crazy how much of a bond you can make in a 12-hour shift with patients and their family members. I have always loved that aspect of my job.
A lot of these patients with the coronavirus are a lot sicker than our normal ICU care, and with no visitors allowed, they are really isolated. But we’ve still gotten to make some really close connections with patients—and family members, even though we can’t meet them in person. When someone’s not having a positive outcome and you’re the only person there with them in end-of-life care, it’s a very powerful moment. Then you’re able to tell their family, ‘I cared about them. I was with them. They weren’t alone.’

I want the families to know we are giving everything that we have to their loved ones.
Rebekah Booth
I want the families to know we are giving everything that we have to their loved ones. We don’t just look at a patient as being a patient in the bed. We look at them as someone’s mother, someone’s sister, someone’s daughter, and we really do care for them like they were our own family.
In some of the success stories that we’ve seen, we’ve given people so much care and just think: How can their bodies get better? So it’s such a victory for us, such a happy moment to get someone discharged from the ICU.
— Rebekah Booth, Registered nurse, Baton Rouge General
We knew ‘what was fixing to happen to us’
As the chief of critical care at Baton Rouge General, Dr. Stephen Brierre monitored the coronavirus outbreak from the beginning. He heard stories from friends at hospitals in Seattle and New Orleans. As soon as its first COVID-19 patient was diagnosed in March, the hospital nearly tripled its ICU capacity in a one-week span. In daily talks, Brierre now updates the team on hospital resources and stresses the importance of preserving N95 masks and medications for patients on ventilators. “To see how the team came together, how nurses who didn’t have ICU experience partnered with ICU nurses to increase the number of patients we can care for … There’s a great deal of camaraderie and willingness to help each other. It’s almost as if we were going into a battle, and all the troops are ready for the fight,” he says. “I have known a lot of rewarding things in my career, but this has been the most rewarding of all of them.”
‘The last thing we want to do is put someone on a ventilator’
Patients with underlying health conditions usually have a harder time coming off ventilators, says Baton Rouge General respiratory therapist Ashley Joffrion. Most patients on ventilators also need to be heavily sedated or chemically paralyzed. And since there’s also a greater need for ventilators right now, Joffrion and her team first try alternate therapies to help with oxygenation, such as noninvasive BiPAP and CPAP machines. “Once we’ve maxed out those therapies,” she says, “that’s when we put them on the ventilator.”
This article was originally part of the June 2020 cover story of 225 Magazine.
|
|
|